Blog
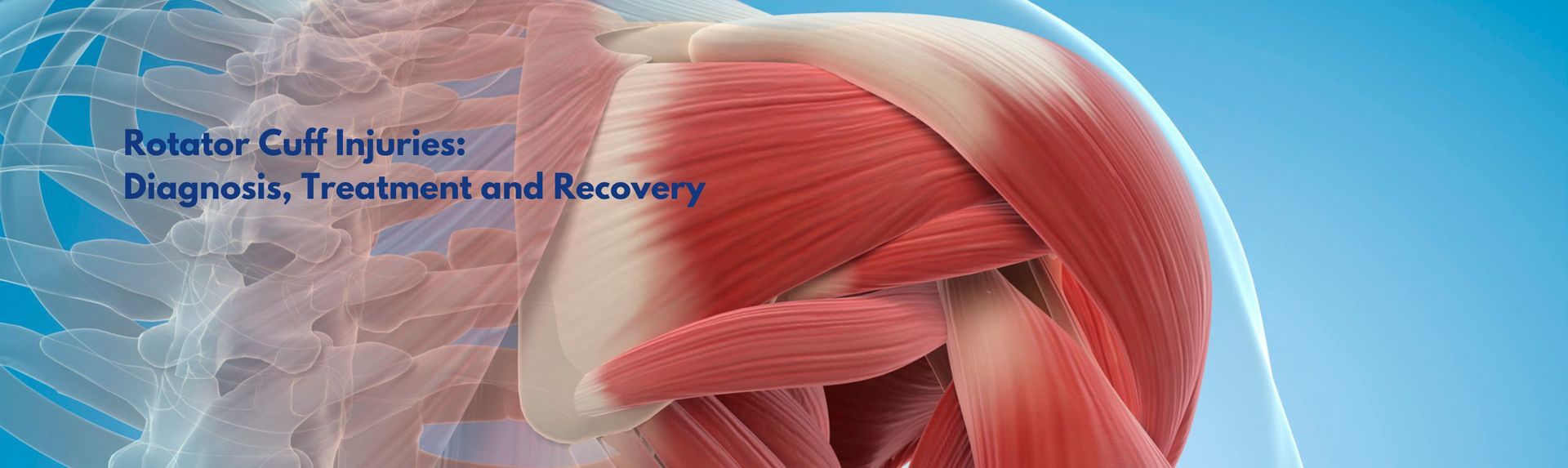
The shoulder is the most mobile joint in the human body —but with that mobility comes a higher risk of injury. At the core of shoulder stability is the rotator cuff , a group of muscles and tendons essential for lifting, reaching, and rotating the arm. Rotator cuff injuries are one of the leading causes of shoulder pain, particularly in people over 40 , athletes, tradies, and anyone performing frequent overhead activities. With early diagnosis and the right treatment plan, many patients return to full function—whether through non-operative care or surgical repair. What Is the Rotator Cuff? The rotator cuff consists of four key muscles and their associated tendons: Supraspinatus Infraspinatus Subscapularis Teres minor These muscles stabilise the shoulder joint and enable controlled arm movement. Injuries to the rotator cuff can range from inflammation and degeneration (tendinopathy) to partial or full-thickness tears . 📊 Clinical Insight : Studies estimate that rotator cuff tears affect 20–30% of adults over age 60 , and that rate increases with age [1]. Causes of Rotator Cuff Injury Degenerative wear and tear (age-related tendon breakdown) Acute trauma , such as a fall or lifting a heavy load Repetitive strain , especially in athletes or manual workers Subacromial impingement , where tendons are compressed under the acromion (part of the shoulder blade) Symptoms of Rotator Cuff Injury Dull or aching pain in the shoulder Pain that worsens at night or when lying on the affected side Difficulty lifting the arm or reaching overhead Weakness when rotating or lifting objects Clicking or catching sensations with movement Symptoms may develop gradually or follow a specific injury. Left untreated, rotator cuff tears can worsen, affecting shoulder stability and long-term function. Diagnosing a Rotator Cuff Injury The first step is a clinical assessment by an orthopaedic surgeon. Dr Ryan du Sart evaluates: Shoulder range of motion Strength and function Pain with specific movements Imaging May Include: Ultrasound – to assess tendon integrity X-ray – to detect bone spurs or joint narrowing MRI – for detailed evaluation of tendon tears or degeneration 📈 Best Practice : Imaging helps differentiate between tendinopathy, partial tears, and complete tendon ruptures , guiding the most appropriate treatment plan [2]. Treatment Options Non-Surgical Management Many rotator cuff injuries—particularly tendinopathy or partial tears—can be managed successfully without surgery. Conservative treatment may include: Activity modification to avoid aggravating movements Physiotherapy to restore strength and shoulder mechanics Anti-inflammatory medication or pain relief Corticosteroid injections for short-term inflammation and pain control These measures are often effective in improving function and reducing pain in less severe injuries. Surgical Treatment Surgery may be recommended when: There is a full-thickness tear or significant tendon damage Symptoms do not improve with conservative care There is functional weakness or loss of motion affecting daily life The tear is acute and linked to trauma in younger, active patients Surgical options include arthroscopic rotator cuff repair , where small incisions and a camera are used to visualise the shoulder and reattach the torn tendon to the bone. This minimally invasive technique reduces soft tissue disruption and promotes faster healing compared to traditional open surgery. Dr du Sart will guide you through the surgical decision-making process and ensure the approach is tailored to your specific goals and lifestyle. Recovery After Surgery Recovery from rotator cuff surgery is a gradual process and involves several phases: Weeks 0–6: Immobilisation with a sling Early passive movement under physiotherapy supervision Pain relief and wound care Weeks 6–12: Begin active range of motion exercises Restore flexibility and shoulder mechanics Start gentle strengthening work Months 3–6: Return to light work or daily activities Continued strengthening and functional retraining Return to sport or overhead work by 6 months , depending on healing and activity level 📊 Evidence-Based Insight : A 2022 meta-analysis reported over 85% success rates for arthroscopic rotator cuff repairs, especially when physiotherapy is properly followed [3]. Shoulder Care Close to Home Dr Ryan du Sart offers comprehensive care for shoulder injuries, from diagnosis through to post-operative rehabilitation. Whether you’re dealing with new shoulder pain or have been managing ongoing symptoms, expert assessment can help clarify your options and restore your shoulder health. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Yamamoto A, Takagishi K, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. Seitz AL, et al. Clinical practice guidelines for the management of rotator cuff disorders. Br J Sports Med. 2019;53(6):305–310. Saccomanno MF, et al. Clinical outcomes and retear rates after rotator cuff repair using a single-row vs double-row technique: a meta-analysis. J Shoulder Elbow Surg. 2022;31(2):351–362.

If you’ve noticed a bump forming at the base of your big toe or pain that makes it difficult to wear certain shoes, you might be dealing with a bunion — a common but often misunderstood foot condition. Bunions can start small but tend to worsen over time, gradually changing the alignment of your toe and affecting the way you walk. The good news? Modern orthopaedic treatments — including advanced surgical options — can relieve pain and restore function so you can get back on your feet comfortably. What Is a Bunion? A bunion (or hallux valgus ) is a bony bump that forms when the big toe drifts towards the smaller toes. This shift puts pressure on the joint, leading to inflammation, pain, and swelling. Over time, the deformity can become more noticeable and may make it hard to find comfortable footwear. In some cases, bunions can also cause corns, calluses, or overlapping toes. Why Bunions Develop There’s no single cause of bunions — but several factors can increase your risk: Family history: Bunions often run in families due to inherited foot structure. Footwear: Tight or narrow shoes, especially those with pointed toes or high heels, can worsen existing deformities. Flat feet or joint laxity: Certain foot shapes place more stress on the big toe joint. Arthritis: Degenerative or inflammatory joint changes can also contribute to bunion formation. When to See a Specialist You don’t need to wait until your bunion becomes severe to seek help. Consider seeing a specialist if you experience: Ongoing pain or swelling around the big toe joint Difficulty finding shoes that fit comfortably Restricted movement of your big toe A visible change in toe alignment Addressing bunions early can help prevent long-term joint damage and improve your comfort during daily activities. Treatment Options Bunion treatment depends on how advanced the deformity is and how much it affects your lifestyle. Non-surgical options may include: Wearing wider, supportive footwear Using padding or orthotics to reduce pressure Taking anti-inflammatory medication as needed Using ice or rest for short-term symptom relief If these measures no longer control your symptoms or the bunion continues to progress, surgical correction may be recommended. Modern bunion surgery focuses on realigning the bones and restoring normal joint function. Procedures are often performed as day surgery, and many patients can bear weight on their foot soon after. Recovery times vary depending on the complexity of the correction, but most people return to normal activities within weeks to months. The Benefits of Specialist Care Seeing an orthopaedic foot and ankle specialist ensures you receive an accurate diagnosis and a treatment plan tailored to your needs. Dr Ryan du Sart uses evidence-based techniques and modern surgical approaches to achieve long-lasting results and faster recovery for his patients. He will assess your bunion, discuss conservative and surgical options, and guide you through what to expect before and after treatment. How to Book an Appointment Dr Ryan du Sart consults at Brecken Health Care in South Bunbury . To see Dr du Sart, simply ask your GP for a referral — it’s a quick and easy process. Early assessment can make a big difference in managing bunion pain and preventing further joint changes. If your bunion is affecting your comfort or mobility, talk to your GP about a referral today. Book Your Appointment Today Your first appointment is the start of your recovery journey—and we’re here to help make it a confident one. 📞 Call (08) 9779 9767 🌐 Book Online at www.ryandusart.com.au 📍 South Bunbury & Busselt o n, WA

Your guide to getting the most out of your orthopaedic consultation in Bunbury or Busselton. Booking your first appointment with an orthopaedic surgeon can feel overwhelming—especially if you're dealing with ongoing joint pain, an injury, or have been told you might need surgery. At Dr Ryan du Sart’s clinics in Bunbury and Busselton , we want you to feel supported, informed, and confident from the very first step. This guide will walk you through what to expect during your consultation and how to prepare—so you can make the most of your visit. Who Is Dr Ryan du Sart? Dr Ryan du Sart is a specialist orthopaedic surgeon with a special interest in joint replacement , foot and ankle conditions , sports injuries , and minimally invasive surgery . He consults across the South West of WA, offering expert orthopaedic care tailored to your individual goals and needs. 📍 Consulting Rooms : Bunbury and Busselton 🌐 www.ryandusart.com.au 📞 Call: (08) 9779 9767 W hy It’s Helpful to Prepare for Your Appointment Taking time to prepare helps you: Feel less anxious about your consultation Ensure all your medical information is available for review Make the most of your time with Dr du Sart Get answers to the questions that matter most to you Before Your Appointment: What to Bring To streamline your visit, please bring: ✅ Referral letter from your GP or specialist ✅ Imaging and reports (X-ray, MRI, CT scans) ✅ Completed patient forms , if provided in advance ✅ Medication list , including prescriptions and supplements ✅ Private health insurance details , if applicable ✅ Loose-fitting clothing so the affected joint can be easily assessed ✅ A list of questions or concerns you’d like to discuss 📌 Tip: Write your symptoms down beforehand—including when they started, what aggravates them, and how they’ve affected your daily life. What to Expect During Your Consultation Your first visit with Dr du Sart typically includes: 1. Medical History: A discussion about your symptoms, past injuries, general health, and any previous treatments or therapies. 2. Physical Examination: An assessment of your joint’s range of motion, strength, stability, and function. 3. Review of Imaging: If you've brought scans or reports, Dr du Sart will go through these with you to help explain what’s happening inside the joint. 4. Diagnosis and Treatment Plan : You’ll receive a clear explanation of your condition, along with tailored recommendations. These may include: Non-surgical options like physiotherapy, medication, or activity modification Injections, bracing, or other supportive care Surgical treatment (if necessary), with information about risks, recovery, and expected outcomes 5. Surgical Planning (If Applicable) If surgery is being considered, Dr du Sart will explain: What the procedure involves Recovery timeframes and rehabilitation How to prepare before and after surgery Use of technology (e.g. robotic-assisted surgery, mymobility® app) Questions You May Want to Ask What is causing my pain or limitation? Are there conservative options I can try before surgery? What are the risks and benefits of surgical treatment? How long is recovery time? Will I need physiotherapy? What lifestyle changes should I make before/after treatment? Asking questions helps ensure you’re comfortable and informed about your next steps. Streamlining Your Experience Dr du Sart’s team aims to make your experience as smooth as possible. You’ll meet friendly staff and may be introduced to other health professionals involved in your care (e.g. physiotherapists or surgical coordinators). We also provide resources like: The mymobility® app to support your recovery depending on the type of surgery you’ve had Information sheets on conditions like knee replacement, ankle surgery, or bunions Ongoing support before and after surgery When You Should Book an Appointment If you’re experiencing: Persistent joint, foot, or ankle pain Limited movement or stiffness Recurrent injuries or instability A recent sports injury Worsening arthritis symptoms ...it may be time to consult a specialist. Why Patients Choose Dr du Sart Patient-first approach with a strong emphasis on education and long-term outcomes Expertise in minimally invasive and robotic-assisted joint surgery Local care with state-of-the-art support in Bunbury and Busselton A focus on making your orthopaedic journey as smooth and stress-free as possible Book Your Appointment Today To book your consultation or find out more: 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, Western Australia Taking the first step toward recovery starts with the right support. Let’s make it a confident one—together.

Bunions (hallux valgus) are a common and often progressive foot condition that can cause significant discomfort, footwear challenges, and interference with daily activities. While early management focuses on non-surgical options, bunion surgery becomes necessary for many patients when pain and deformity worsen despite conservative care. This guide will help you understand when to consider surgery, what’s involved, and what recovery looks like. What Is a Bunion? A bunion is a bony bump that develops at the base of the big toe , causing the toe to drift toward the second toe. This misalignment can lead to joint inflammation, swelling, pain, and difficulty finding comfortable shoes. Contributing Factors: Genetics and inherited foot shape Poorly fitting shoes , particularly narrow or high-heeled styles Flat feet or hypermobility Arthritis and joint degeneration A related condition, the bunionette , affects the outer edge of the foot at the fifth toe . 📊 Clinical Insight : Bunions are more common in women and can affect up to 23% of adults aged 18–65 , and over 35% in people aged 65 and older [1]. When Should You Consider Surgery? Surgery may be appropriate when: Pain persists despite using orthotics or changing footwear Your bunion limits your ability to walk, work, or enjoy activities There is increasing deformity, stiffness, or joint instability Other toes (e.g. the second toe) are becoming affected You’re experiencing skin irritation or pressure sores Delaying surgical intervention can increase the risk of toe deformities, chronic pain, or irreversible joint damage . Dr Ryan du Sart’s Approach to Bunion Surgery Dr du Sart performs minimally invasive (keyhole) bunion surgery , which uses smaller incisions and targeted correction, resulting in: Less disruption to soft tissue Lower post-operative pain and swelling Faster recovery than traditional open techniques Procedure Overview: Tiny incisions are made near the base of the big toe A burr is used to perform precise osteotomies (bone cuts) of the 1st metatarsal and proximal phalanx Bones are realigned to correct the deformity Zero-profile screws are used for fixation, minimising hardware prominence Soft tissue balancing and joint alignment are refined for better long-term function This technique is suitable for most patients with mild to moderate bunion deformities and delivers both cosmetic and mechanical improvements. 📈 Evidence-Based Outcome : Studies have shown that minimally invasive bunion surgery is associated with high patient satisfaction, quicker return to footwear, and lower complication rates compared to traditional open procedures [2]. Benefits of Minimally Invasive Bunion Surgery ✅ Smaller incisions and minimal scarring ✅ Shorter recovery time and less swelling ✅ Less post-operative discomfort ✅ Early return to shoes and daily activity ✅ Improved joint mechanics and long-term alignment Recovery After Bunion Surgery Post-Operative Care Walking is permitted immediately in a surgical shoe Elevation is key during the first 1–2 weeks to manage swelling Crutches may be used initially for support Transition to supportive sneakers typically occurs at 3 weeks Gentle mobility and toe-strengthening exercises begin early Return to Activity Light desk-based work: 2–3 weeks Standing or walking jobs: 4–6 weeks Heavy physical activity or sport: 8–12 weeks Full recovery: 6–12 months , depending on healing and activity level Driving Right foot: Wait 6 weeks minimum Left foot (automatic car): May return sooner with surgeon clearance 📊 Tip : Most patients report a significant reduction in pain and improvement in foot shape and function within 8–12 weeks . Is Bunion Surgery Right for You? The decision to proceed with surgery is highly individual. During your consultation, Dr du Sart will: Assess your medical history, symptoms, and functional limitations Review any imaging (e.g. X-rays) Discuss your lifestyle, footwear needs, and activity goals Explain surgical options and expected recovery A Personalised Approach, Close to Home Dr Ryan du Sart consults in Bunbury and Busselton , providing modern orthopaedic foot and ankle care to patients throughout the South West region. From initial diagnosis to post-operative rehabilitation, his approach is tailored to ensure the best possible outcome for each individual. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3(1):21. Redfern D, Perera A, Dagneaux L. Minimally invasive surgery for hallux valgus: A systematic review and meta-analysis. EFORT Open Rev. 2020;5(8):512–520.

Shoulder arthritis is a progressive condition that can interfere with daily tasks like reaching, dressing, sleeping, and even simple lifting movements. While it receives less attention than hip or knee arthritis, it can significantly impact function, comfort, and independence —especially in older adults. At Dr Ryan du Sart’s orthopaedic practice in Bunbury and Busselton, we help patients manage shoulder arthritis using a personalised approach focused on pain relief, movement preservation, and surgical intervention when needed. What Is Shoulder Arthritis? Shoulder arthritis occurs when the cartilage lining the shoulder joint wears away , causing the bones to rub against each other. This leads to pain, inflammation, stiffness, and eventually, reduced range of motion. Over time, shoulder arthritis can significantly limit function, making it harder to perform daily tasks such as washing hair, reaching for items on shelves, or sleeping comfortably. There are several types of shoulder arthritis, including: Osteoarthritis (degenerative wear and tear) Rheumatoid arthritis (inflammatory) Post-traumatic arthritis (after injury) Cuff tear arthropathy (from massive, chronic rotator cuff tears) 📊 Clinical Note : Shoulder osteoarthritis affects approximately 16% of adults over the age of 65 , and incidence increases significantly after 70 [1]. Common Symptoms Deep or aching shoulder pain Pain that worsens with activity or at night Limited range of motion Stiffness and difficulty with overhead tasks Weakness, especially with lifting or rotating the arm A grinding, catching, or popping sensation Symptoms typically progress gradually. Many patients mistakenly assume their pain is due to ageing—but early diagnosis can lead to better outcomes . Non-Surgical Management For many patients, shoulder arthritis can be effectively managed without surgery—especially in the early to moderate stages. Lifestyle and Activity Modifications Avoid heavy lifting or repetitive overhead activities Use the non-affected arm for demanding tasks Modify workstations or daily routines to reduce joint stress Medications Paracetamol or Panadol Osteo for mild to moderate pain NSAIDs (e.g. ibuprofen, meloxicam) if tolerated Topical anti-inflammatory gels as a local pain relief option Always consult your GP to ensure medications are safe for your health profile. Physiotherapy Gentle range-of-motion exercises to reduce stiffness Strength training of shoulder and scapular muscles Postural correction and functional movement retraining 📈 Evidence Insight : A 2021 review confirmed that structured physiotherapy significantly improves pain and function in early-stage glenohumeral OA [2]. Cortisone Injections Cortisone injections can reduce inflammation and provide short-term relief (weeks to months) Most effective in moderate cases or when flare-ups occur Typically offered no more than 3 times per year When Is Surgery Considered? Surgery may be considered if: Pain limits sleep, daily activity, or work Imaging shows severe cartilage loss or joint changes You’ve trialled conservative care without improvement There is a large or irreparable rotator cuff tear Shoulder Arthroscopy A minimally invasive “clean out” procedure to remove loose bodies, smooth damaged cartilage, or address bursitis. Suitable for mild to moderate arthritis or diagnostic purposes. Shoulder Replacement Surgery When arthritis is advanced, joint replacement may be the most effective treatment. Options include: Total Shoulder Replacement (TSR) : Ideal when the rotator cuff is intact Reverse Shoulder Replacement (RSR) : Used when rotator cuff function is compromised 📊 Outcomes Insight : Both procedures have shown over 90% satisfaction rates for reducing pain and improving function when performed at the right stage [3]. Recovery After Surgery First 2–6 weeks : Sling use, wound care, and pain management Weeks 6–12 : Begin active movement and structured physiotherapy Months 3–6 : Regain strength, range of motion, and functional capacity Full recovery may take 4–6 months , with improvements continuing for up to a year Dr du Sart’s patients receive a detailed rehab plan and support throughout the recovery journey. Shoulder Pain Isn’t Just “Getting Older” Too many patients live with treatable shoulder arthritis, assuming it’s a normal part of ageing. But shoulder arthritis is a diagnosable and manageable condition , and there are evidence-based strategies that can help. If your shoulder pain is affecting sleep, work, or quality of life—it’s time to explore your options. Orthopaedic Shoulder Care in the South West Dr Ryan du Sart provides comprehensive shoulder assessments and personalised treatment options, with a focus on patient education and long-term outcomes. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Chillemi C, et al. Epidemiology and risk factors of degenerative shoulder diseases. Musculoskelet Surg. 2011;95(Suppl 1):S49–S59. Thomas T, et al. Effectiveness of conservative treatment strategies in glenohumeral osteoarthritis: a systematic review. Physiother Theory Pract. 2021;37(8):893–903. Bohsali KI, et al. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(10):2279–2292.

Chronic shoulder pain, stiffness, and loss of function can have a profound effect on your independence, sleep, and quality of life. For many patients, shoulder pain builds gradually over time and is often related to degenerative conditions like arthritis or long-standing rotator cuff injuries. While many shoulder conditions can be managed with conservative treatment, shoulder replacement surgery may become necessary when pain persists, mobility declines, and other treatments no longer provide relief. In this article, we’ll explore the key signs that it may be time to consider shoulder replacement, what the procedure involves, and how to take the next step. What Is Shoulder Replacement Surgery? Shoulder replacement (arthroplasty) involves removing damaged parts of the shoulder joint and replacing them with prosthetic components. It is a highly effective treatment for advanced arthritis and rotator cuff-related degeneration , providing substantial pain relief and restoring function. There are two main types: Total Shoulder Replacement (Anatomic): Replaces both the humeral head (ball) and glenoid (socket). Suitable when the rotator cuff tendons are intact . Reverse Total Shoulder Replacement: Reverses the ball-and-socket configuration. Indicated for massive rotator cuff tears, cuff tear arthropathy , or complex arthritis. This design shifts movement mechanics to the deltoid muscle , compensating for rotator cuff dysfunction. 📈 Evidence Insight : According to a 2020 registry review, shoulder replacements have over 90% satisfaction rates and can last 15–20 years in many patients [1]. Signs It May Be Time for Shoulder Replacement Surgery Severe, Persistent Shoulder Pain: Pain that disrupts sleep, limits daily activities, or is present at rest may signal the need for surgical intervention. Advanced Shoulder Arthritis: X-rays and imaging may show joint space narrowing, bone-on-bone contact, bone spurs, or structural deformity of the joint, confirming arthritis progression. Stiffness and Limited Range of Motion: When conservative treatments no longer restore mobility, and everyday tasks like dressing, reaching overhead, or washing your hair become difficult, surgery may be the next step. Failed Non-Surgical Treatments: If medications, physiotherapy, injections, and activity modification no longer provide lasting relief, surgical intervention may offer more effective long-term outcomes. Large or Irreparable Rotator Cuff Tears: In cases where the rotator cuff is severely torn or no longer functioning (cuff tear arthropathy), a reverse shoulder replacement may be recommended to restore stability and function. When to Talk to a Specialist If shoulder pain has become a daily limitation, early referral for an orthopaedic evaluation is recommended. Dr Ryan du Sart will assess: Joint condition via physical exam and imaging Muscle integrity and rotator cuff status Your lifestyle, activity level , and treatment goals 📊 Clinical Note : Early assessment can often delay or optimise the timing of surgery. A 2021 study found patients undergoing surgery at the appropriate stage reported better functional outcomes and fewer complications [2]. What Does Recovery Look Like? Shoulder replacement is a major procedure, but outcomes are generally very positive when performed at the right time and followed by structured rehabilitation. Recovery timeline: 0–6 weeks: Shoulder supported in a sling; early physiotherapy to maintain motion 6–12 weeks: Gradual increase in active movement and strength 3–6 months: Return to light daily activities and driving 6–12 months: Full recovery for most patients, including return to recreation and improved sleep Dr du Sart and his team will support you throughout your recovery with tailored rehab plans and regular follow-up. Why Choose Dr Ryan du Sart Dr du Sart is an experienced orthopaedic surgeon with a patient-first approach, offering shoulder replacement surgery to patients throughout the South West of WA. With consulting rooms in Bunbury and Busselton , he provides local access to advanced orthopaedic care without the need to travel far from home. His focus is on: Evidence-based, personalised treatment Minimally invasive and joint-preserving techniques where possible Long-term outcomes and quality of life 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2020 . Saltzman BM, et al. Impact of surgical timing on outcomes in shoulder arthroplasty for osteoarthritis: A matched cohort study . J Shoulder Elbow Surg. 2021;30(5):1127–1135.

By Dr Ryan du Sart – Orthopaedic Surgeon, South West WA If you're preparing for orthopaedic surgery with Dr Ryan du Sart, it’s completely natural to feel a mix of anticipation and nerves. Understanding what will happen on the day of your procedure can ease anxiety, help you feel more confident, and ensure a smooth experience from arrival to discharge. Whether you're undergoing a joint replacement , arthroscopy , or foot and ankle surgery , this step-by-step guide outlines what to expect on your surgery day. 1. Before You Arrive In the days leading up to your procedure, you’ll receive detailed instructions from Dr du Sart’s team, including: Admission time and hospital location Fasting guidelines (typically no food or drink 6–8 hours prior to surgery) Medications to pause or continue What to bring: comfortable clothing, your hospital paperwork, Medicare and private health details If you’re using the mymobility® app, ensure your phone is charged and accessible—you’ll be able to track recovery milestones post-operatively. 2. Hospital Check-In Upon arrival at the hospital: You’ll check in with the admissions team A nurse will confirm your details, check vital signs, and prepare you for theatre An anaesthetist will meet with you to discuss your anaesthetic plan (general, spinal, or local) Dr du Sart will review the procedure with you and answer any last-minute questions You’ll be asked to change into a surgical gown and remove any jewellery, nail polish, or contact lenses. 3. Heading to the Operating Theatre When it’s time for your surgery: You’ll be taken to the pre-operative area A member of the surgical team will guide you into the operating theatre Anaesthesia is administered under close monitoring Dr du Sart will perform your surgery using modern, evidence-based techniques tailored to your condition Surgery times vary by procedure—for example, a knee arthroscopy may take under an hour, while a joint replacement can take 1.5–2 hours. 4. Waking Up in Recovery After surgery, you’ll be taken to the post-anaesthesia care unit (PACU) where: Nurses will monitor your vital signs, pain, and surgical site You may have a drip (IV) in place, and possibly a bandage, splint, or brace Pain will be managed using medications as needed Once you’re fully awake and stable, you’ll be transferred to your hospital room. 5. After Surgery: Your Hospital Stay Depending on your procedure, you may: Go home the same day (day surgery or minor procedures), or Stay overnight (e.g. for joint replacement or ligament repair) While in hospital: You’ll be encouraged to move (usually with assistance) as soon as possible Physiotherapists will visit to begin rehabilitation exercises You’ll receive post-operative instructions , including pain relief, wound care, and activity restrictions For joint replacements, the use of the Game Ready® system may also help reduce swelling and discomfort during the early recovery phase. 6. Going Home and Recovery Before discharge: You’ll be given a summary of your procedure Discharge instructions and follow-up appointments will be arranged Prescriptions for pain relief or anti-inflammatories will be provided You’ll receive guidance on when to resume walking, showering, and normal activities Expect a follow-up review with Dr du Sart typically 10–14 days after surgery. Depending on the surgery you’ve had you may be referred to the mymobility® app. This app will help guide your daily recovery with customised exercises, reminders, and educational content. Tips for a Smooth Experience ✅ Organise transport home in advance ✅ Arrange support for cooking, cleaning, and mobility if needed ✅ Follow medication and fasting instructions exactly ✅ Ask questions —our team is here to help ✅ Keep moving (within limits) after surgery to support circulation and healing You’re in Expert Hands Dr Ryan du Sart is committed to delivering high-quality orthopaedic care using modern, minimally invasive techniques and technology. With clinics in Bunbury and Busselton , we aim to make your surgical experience as safe, comfortable, and well-supported as possible. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA Surgery can be a l ife-changing step toward pain relief and restored mobility. With the right preparation and support, your journey starts with confidence—and ends with better movement.
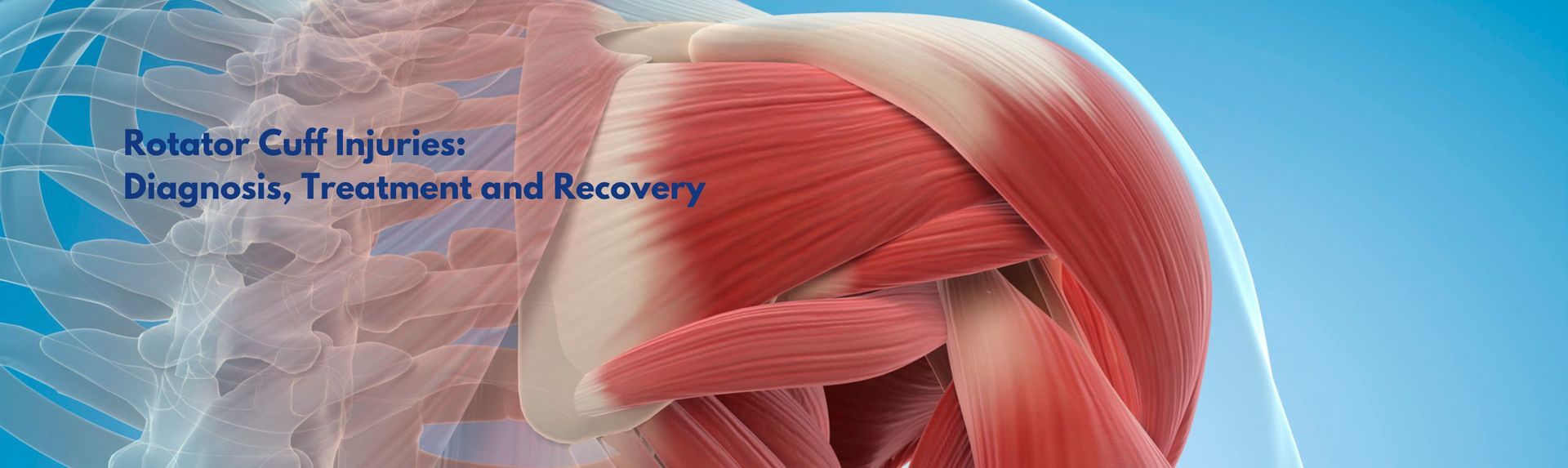
The shoulder is the most mobile joint in the human body —but with that mobility comes a higher risk of injury. At the core of shoulder stability is the rotator cuff , a group of muscles and tendons essential for lifting, reaching, and rotating the arm. Rotator cuff injuries are one of the leading causes of shoulder pain, particularly in people over 40 , athletes, tradies, and anyone performing frequent overhead activities. With early diagnosis and the right treatment plan, many patients return to full function—whether through non-operative care or surgical repair. What Is the Rotator Cuff? The rotator cuff consists of four key muscles and their associated tendons: Supraspinatus Infraspinatus Subscapularis Teres minor These muscles stabilise the shoulder joint and enable controlled arm movement. Injuries to the rotator cuff can range from inflammation and degeneration (tendinopathy) to partial or full-thickness tears . 📊 Clinical Insight : Studies estimate that rotator cuff tears affect 20–30% of adults over age 60 , and that rate increases with age [1]. Causes of Rotator Cuff Injury Degenerative wear and tear (age-related tendon breakdown) Acute trauma , such as a fall or lifting a heavy load Repetitive strain , especially in athletes or manual workers Subacromial impingement , where tendons are compressed under the acromion (part of the shoulder blade) Symptoms of Rotator Cuff Injury Dull or aching pain in the shoulder Pain that worsens at night or when lying on the affected side Difficulty lifting the arm or reaching overhead Weakness when rotating or lifting objects Clicking or catching sensations with movement Symptoms may develop gradually or follow a specific injury. Left untreated, rotator cuff tears can worsen, affecting shoulder stability and long-term function. Diagnosing a Rotator Cuff Injury The first step is a clinical assessment by an orthopaedic surgeon. Dr Ryan du Sart evaluates: Shoulder range of motion Strength and function Pain with specific movements Imaging May Include: Ultrasound – to assess tendon integrity X-ray – to detect bone spurs or joint narrowing MRI – for detailed evaluation of tendon tears or degeneration 📈 Best Practice : Imaging helps differentiate between tendinopathy, partial tears, and complete tendon ruptures , guiding the most appropriate treatment plan [2]. Treatment Options Non-Surgical Management Many rotator cuff injuries—particularly tendinopathy or partial tears—can be managed successfully without surgery. Conservative treatment may include: Activity modification to avoid aggravating movements Physiotherapy to restore strength and shoulder mechanics Anti-inflammatory medication or pain relief Corticosteroid injections for short-term inflammation and pain control These measures are often effective in improving function and reducing pain in less severe injuries. Surgical Treatment Surgery may be recommended when: There is a full-thickness tear or significant tendon damage Symptoms do not improve with conservative care There is functional weakness or loss of motion affecting daily life The tear is acute and linked to trauma in younger, active patients Surgical options include arthroscopic rotator cuff repair , where small incisions and a camera are used to visualise the shoulder and reattach the torn tendon to the bone. This minimally invasive technique reduces soft tissue disruption and promotes faster healing compared to traditional open surgery. Dr du Sart will guide you through the surgical decision-making process and ensure the approach is tailored to your specific goals and lifestyle. Recovery After Surgery Recovery from rotator cuff surgery is a gradual process and involves several phases: Weeks 0–6: Immobilisation with a sling Early passive movement under physiotherapy supervision Pain relief and wound care Weeks 6–12: Begin active range of motion exercises Restore flexibility and shoulder mechanics Start gentle strengthening work Months 3–6: Return to light work or daily activities Continued strengthening and functional retraining Return to sport or overhead work by 6 months , depending on healing and activity level 📊 Evidence-Based Insight : A 2022 meta-analysis reported over 85% success rates for arthroscopic rotator cuff repairs, especially when physiotherapy is properly followed [3]. Shoulder Care Close to Home Dr Ryan du Sart offers comprehensive care for shoulder injuries, from diagnosis through to post-operative rehabilitation. Whether you’re dealing with new shoulder pain or have been managing ongoing symptoms, expert assessment can help clarify your options and restore your shoulder health. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Yamamoto A, Takagishi K, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. Seitz AL, et al. Clinical practice guidelines for the management of rotator cuff disorders. Br J Sports Med. 2019;53(6):305–310. Saccomanno MF, et al. Clinical outcomes and retear rates after rotator cuff repair using a single-row vs double-row technique: a meta-analysis. J Shoulder Elbow Surg. 2022;31(2):351–362.

If you’ve noticed a bump forming at the base of your big toe or pain that makes it difficult to wear certain shoes, you might be dealing with a bunion — a common but often misunderstood foot condition. Bunions can start small but tend to worsen over time, gradually changing the alignment of your toe and affecting the way you walk. The good news? Modern orthopaedic treatments — including advanced surgical options — can relieve pain and restore function so you can get back on your feet comfortably. What Is a Bunion? A bunion (or hallux valgus ) is a bony bump that forms when the big toe drifts towards the smaller toes. This shift puts pressure on the joint, leading to inflammation, pain, and swelling. Over time, the deformity can become more noticeable and may make it hard to find comfortable footwear. In some cases, bunions can also cause corns, calluses, or overlapping toes. Why Bunions Develop There’s no single cause of bunions — but several factors can increase your risk: Family history: Bunions often run in families due to inherited foot structure. Footwear: Tight or narrow shoes, especially those with pointed toes or high heels, can worsen existing deformities. Flat feet or joint laxity: Certain foot shapes place more stress on the big toe joint. Arthritis: Degenerative or inflammatory joint changes can also contribute to bunion formation. When to See a Specialist You don’t need to wait until your bunion becomes severe to seek help. Consider seeing a specialist if you experience: Ongoing pain or swelling around the big toe joint Difficulty finding shoes that fit comfortably Restricted movement of your big toe A visible change in toe alignment Addressing bunions early can help prevent long-term joint damage and improve your comfort during daily activities. Treatment Options Bunion treatment depends on how advanced the deformity is and how much it affects your lifestyle. Non-surgical options may include: Wearing wider, supportive footwear Using padding or orthotics to reduce pressure Taking anti-inflammatory medication as needed Using ice or rest for short-term symptom relief If these measures no longer control your symptoms or the bunion continues to progress, surgical correction may be recommended. Modern bunion surgery focuses on realigning the bones and restoring normal joint function. Procedures are often performed as day surgery, and many patients can bear weight on their foot soon after. Recovery times vary depending on the complexity of the correction, but most people return to normal activities within weeks to months. The Benefits of Specialist Care Seeing an orthopaedic foot and ankle specialist ensures you receive an accurate diagnosis and a treatment plan tailored to your needs. Dr Ryan du Sart uses evidence-based techniques and modern surgical approaches to achieve long-lasting results and faster recovery for his patients. He will assess your bunion, discuss conservative and surgical options, and guide you through what to expect before and after treatment. How to Book an Appointment Dr Ryan du Sart consults at Brecken Health Care in South Bunbury . To see Dr du Sart, simply ask your GP for a referral — it’s a quick and easy process. Early assessment can make a big difference in managing bunion pain and preventing further joint changes. If your bunion is affecting your comfort or mobility, talk to your GP about a referral today. Book Your Appointment Today Your first appointment is the start of your recovery journey—and we’re here to help make it a confident one. 📞 Call (08) 9779 9767 🌐 Book Online at www.ryandusart.com.au 📍 South Bunbury & Busselt o n, WA

Your guide to getting the most out of your orthopaedic consultation in Bunbury or Busselton. Booking your first appointment with an orthopaedic surgeon can feel overwhelming—especially if you're dealing with ongoing joint pain, an injury, or have been told you might need surgery. At Dr Ryan du Sart’s clinics in Bunbury and Busselton , we want you to feel supported, informed, and confident from the very first step. This guide will walk you through what to expect during your consultation and how to prepare—so you can make the most of your visit. Who Is Dr Ryan du Sart? Dr Ryan du Sart is a specialist orthopaedic surgeon with a special interest in joint replacement , foot and ankle conditions , sports injuries , and minimally invasive surgery . He consults across the South West of WA, offering expert orthopaedic care tailored to your individual goals and needs. 📍 Consulting Rooms : Bunbury and Busselton 🌐 www.ryandusart.com.au 📞 Call: (08) 9779 9767 W hy It’s Helpful to Prepare for Your Appointment Taking time to prepare helps you: Feel less anxious about your consultation Ensure all your medical information is available for review Make the most of your time with Dr du Sart Get answers to the questions that matter most to you Before Your Appointment: What to Bring To streamline your visit, please bring: ✅ Referral letter from your GP or specialist ✅ Imaging and reports (X-ray, MRI, CT scans) ✅ Completed patient forms , if provided in advance ✅ Medication list , including prescriptions and supplements ✅ Private health insurance details , if applicable ✅ Loose-fitting clothing so the affected joint can be easily assessed ✅ A list of questions or concerns you’d like to discuss 📌 Tip: Write your symptoms down beforehand—including when they started, what aggravates them, and how they’ve affected your daily life. What to Expect During Your Consultation Your first visit with Dr du Sart typically includes: 1. Medical History: A discussion about your symptoms, past injuries, general health, and any previous treatments or therapies. 2. Physical Examination: An assessment of your joint’s range of motion, strength, stability, and function. 3. Review of Imaging: If you've brought scans or reports, Dr du Sart will go through these with you to help explain what’s happening inside the joint. 4. Diagnosis and Treatment Plan : You’ll receive a clear explanation of your condition, along with tailored recommendations. These may include: Non-surgical options like physiotherapy, medication, or activity modification Injections, bracing, or other supportive care Surgical treatment (if necessary), with information about risks, recovery, and expected outcomes 5. Surgical Planning (If Applicable) If surgery is being considered, Dr du Sart will explain: What the procedure involves Recovery timeframes and rehabilitation How to prepare before and after surgery Use of technology (e.g. robotic-assisted surgery, mymobility® app) Questions You May Want to Ask What is causing my pain or limitation? Are there conservative options I can try before surgery? What are the risks and benefits of surgical treatment? How long is recovery time? Will I need physiotherapy? What lifestyle changes should I make before/after treatment? Asking questions helps ensure you’re comfortable and informed about your next steps. Streamlining Your Experience Dr du Sart’s team aims to make your experience as smooth as possible. You’ll meet friendly staff and may be introduced to other health professionals involved in your care (e.g. physiotherapists or surgical coordinators). We also provide resources like: The mymobility® app to support your recovery depending on the type of surgery you’ve had Information sheets on conditions like knee replacement, ankle surgery, or bunions Ongoing support before and after surgery When You Should Book an Appointment If you’re experiencing: Persistent joint, foot, or ankle pain Limited movement or stiffness Recurrent injuries or instability A recent sports injury Worsening arthritis symptoms ...it may be time to consult a specialist. Why Patients Choose Dr du Sart Patient-first approach with a strong emphasis on education and long-term outcomes Expertise in minimally invasive and robotic-assisted joint surgery Local care with state-of-the-art support in Bunbury and Busselton A focus on making your orthopaedic journey as smooth and stress-free as possible Book Your Appointment Today To book your consultation or find out more: 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, Western Australia Taking the first step toward recovery starts with the right support. Let’s make it a confident one—together.

Bunions (hallux valgus) are a common and often progressive foot condition that can cause significant discomfort, footwear challenges, and interference with daily activities. While early management focuses on non-surgical options, bunion surgery becomes necessary for many patients when pain and deformity worsen despite conservative care. This guide will help you understand when to consider surgery, what’s involved, and what recovery looks like. What Is a Bunion? A bunion is a bony bump that develops at the base of the big toe , causing the toe to drift toward the second toe. This misalignment can lead to joint inflammation, swelling, pain, and difficulty finding comfortable shoes. Contributing Factors: Genetics and inherited foot shape Poorly fitting shoes , particularly narrow or high-heeled styles Flat feet or hypermobility Arthritis and joint degeneration A related condition, the bunionette , affects the outer edge of the foot at the fifth toe . 📊 Clinical Insight : Bunions are more common in women and can affect up to 23% of adults aged 18–65 , and over 35% in people aged 65 and older [1]. When Should You Consider Surgery? Surgery may be appropriate when: Pain persists despite using orthotics or changing footwear Your bunion limits your ability to walk, work, or enjoy activities There is increasing deformity, stiffness, or joint instability Other toes (e.g. the second toe) are becoming affected You’re experiencing skin irritation or pressure sores Delaying surgical intervention can increase the risk of toe deformities, chronic pain, or irreversible joint damage . Dr Ryan du Sart’s Approach to Bunion Surgery Dr du Sart performs minimally invasive (keyhole) bunion surgery , which uses smaller incisions and targeted correction, resulting in: Less disruption to soft tissue Lower post-operative pain and swelling Faster recovery than traditional open techniques Procedure Overview: Tiny incisions are made near the base of the big toe A burr is used to perform precise osteotomies (bone cuts) of the 1st metatarsal and proximal phalanx Bones are realigned to correct the deformity Zero-profile screws are used for fixation, minimising hardware prominence Soft tissue balancing and joint alignment are refined for better long-term function This technique is suitable for most patients with mild to moderate bunion deformities and delivers both cosmetic and mechanical improvements. 📈 Evidence-Based Outcome : Studies have shown that minimally invasive bunion surgery is associated with high patient satisfaction, quicker return to footwear, and lower complication rates compared to traditional open procedures [2]. Benefits of Minimally Invasive Bunion Surgery ✅ Smaller incisions and minimal scarring ✅ Shorter recovery time and less swelling ✅ Less post-operative discomfort ✅ Early return to shoes and daily activity ✅ Improved joint mechanics and long-term alignment Recovery After Bunion Surgery Post-Operative Care Walking is permitted immediately in a surgical shoe Elevation is key during the first 1–2 weeks to manage swelling Crutches may be used initially for support Transition to supportive sneakers typically occurs at 3 weeks Gentle mobility and toe-strengthening exercises begin early Return to Activity Light desk-based work: 2–3 weeks Standing or walking jobs: 4–6 weeks Heavy physical activity or sport: 8–12 weeks Full recovery: 6–12 months , depending on healing and activity level Driving Right foot: Wait 6 weeks minimum Left foot (automatic car): May return sooner with surgeon clearance 📊 Tip : Most patients report a significant reduction in pain and improvement in foot shape and function within 8–12 weeks . Is Bunion Surgery Right for You? The decision to proceed with surgery is highly individual. During your consultation, Dr du Sart will: Assess your medical history, symptoms, and functional limitations Review any imaging (e.g. X-rays) Discuss your lifestyle, footwear needs, and activity goals Explain surgical options and expected recovery A Personalised Approach, Close to Home Dr Ryan du Sart consults in Bunbury and Busselton , providing modern orthopaedic foot and ankle care to patients throughout the South West region. From initial diagnosis to post-operative rehabilitation, his approach is tailored to ensure the best possible outcome for each individual. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3(1):21. Redfern D, Perera A, Dagneaux L. Minimally invasive surgery for hallux valgus: A systematic review and meta-analysis. EFORT Open Rev. 2020;5(8):512–520.

Shoulder arthritis is a progressive condition that can interfere with daily tasks like reaching, dressing, sleeping, and even simple lifting movements. While it receives less attention than hip or knee arthritis, it can significantly impact function, comfort, and independence —especially in older adults. At Dr Ryan du Sart’s orthopaedic practice in Bunbury and Busselton, we help patients manage shoulder arthritis using a personalised approach focused on pain relief, movement preservation, and surgical intervention when needed. What Is Shoulder Arthritis? Shoulder arthritis occurs when the cartilage lining the shoulder joint wears away , causing the bones to rub against each other. This leads to pain, inflammation, stiffness, and eventually, reduced range of motion. Over time, shoulder arthritis can significantly limit function, making it harder to perform daily tasks such as washing hair, reaching for items on shelves, or sleeping comfortably. There are several types of shoulder arthritis, including: Osteoarthritis (degenerative wear and tear) Rheumatoid arthritis (inflammatory) Post-traumatic arthritis (after injury) Cuff tear arthropathy (from massive, chronic rotator cuff tears) 📊 Clinical Note : Shoulder osteoarthritis affects approximately 16% of adults over the age of 65 , and incidence increases significantly after 70 [1]. Common Symptoms Deep or aching shoulder pain Pain that worsens with activity or at night Limited range of motion Stiffness and difficulty with overhead tasks Weakness, especially with lifting or rotating the arm A grinding, catching, or popping sensation Symptoms typically progress gradually. Many patients mistakenly assume their pain is due to ageing—but early diagnosis can lead to better outcomes . Non-Surgical Management For many patients, shoulder arthritis can be effectively managed without surgery—especially in the early to moderate stages. Lifestyle and Activity Modifications Avoid heavy lifting or repetitive overhead activities Use the non-affected arm for demanding tasks Modify workstations or daily routines to reduce joint stress Medications Paracetamol or Panadol Osteo for mild to moderate pain NSAIDs (e.g. ibuprofen, meloxicam) if tolerated Topical anti-inflammatory gels as a local pain relief option Always consult your GP to ensure medications are safe for your health profile. Physiotherapy Gentle range-of-motion exercises to reduce stiffness Strength training of shoulder and scapular muscles Postural correction and functional movement retraining 📈 Evidence Insight : A 2021 review confirmed that structured physiotherapy significantly improves pain and function in early-stage glenohumeral OA [2]. Cortisone Injections Cortisone injections can reduce inflammation and provide short-term relief (weeks to months) Most effective in moderate cases or when flare-ups occur Typically offered no more than 3 times per year When Is Surgery Considered? Surgery may be considered if: Pain limits sleep, daily activity, or work Imaging shows severe cartilage loss or joint changes You’ve trialled conservative care without improvement There is a large or irreparable rotator cuff tear Shoulder Arthroscopy A minimally invasive “clean out” procedure to remove loose bodies, smooth damaged cartilage, or address bursitis. Suitable for mild to moderate arthritis or diagnostic purposes. Shoulder Replacement Surgery When arthritis is advanced, joint replacement may be the most effective treatment. Options include: Total Shoulder Replacement (TSR) : Ideal when the rotator cuff is intact Reverse Shoulder Replacement (RSR) : Used when rotator cuff function is compromised 📊 Outcomes Insight : Both procedures have shown over 90% satisfaction rates for reducing pain and improving function when performed at the right stage [3]. Recovery After Surgery First 2–6 weeks : Sling use, wound care, and pain management Weeks 6–12 : Begin active movement and structured physiotherapy Months 3–6 : Regain strength, range of motion, and functional capacity Full recovery may take 4–6 months , with improvements continuing for up to a year Dr du Sart’s patients receive a detailed rehab plan and support throughout the recovery journey. Shoulder Pain Isn’t Just “Getting Older” Too many patients live with treatable shoulder arthritis, assuming it’s a normal part of ageing. But shoulder arthritis is a diagnosable and manageable condition , and there are evidence-based strategies that can help. If your shoulder pain is affecting sleep, work, or quality of life—it’s time to explore your options. Orthopaedic Shoulder Care in the South West Dr Ryan du Sart provides comprehensive shoulder assessments and personalised treatment options, with a focus on patient education and long-term outcomes. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Chillemi C, et al. Epidemiology and risk factors of degenerative shoulder diseases. Musculoskelet Surg. 2011;95(Suppl 1):S49–S59. Thomas T, et al. Effectiveness of conservative treatment strategies in glenohumeral osteoarthritis: a systematic review. Physiother Theory Pract. 2021;37(8):893–903. Bohsali KI, et al. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(10):2279–2292.

Chronic shoulder pain, stiffness, and loss of function can have a profound effect on your independence, sleep, and quality of life. For many patients, shoulder pain builds gradually over time and is often related to degenerative conditions like arthritis or long-standing rotator cuff injuries. While many shoulder conditions can be managed with conservative treatment, shoulder replacement surgery may become necessary when pain persists, mobility declines, and other treatments no longer provide relief. In this article, we’ll explore the key signs that it may be time to consider shoulder replacement, what the procedure involves, and how to take the next step. What Is Shoulder Replacement Surgery? Shoulder replacement (arthroplasty) involves removing damaged parts of the shoulder joint and replacing them with prosthetic components. It is a highly effective treatment for advanced arthritis and rotator cuff-related degeneration , providing substantial pain relief and restoring function. There are two main types: Total Shoulder Replacement (Anatomic): Replaces both the humeral head (ball) and glenoid (socket). Suitable when the rotator cuff tendons are intact . Reverse Total Shoulder Replacement: Reverses the ball-and-socket configuration. Indicated for massive rotator cuff tears, cuff tear arthropathy , or complex arthritis. This design shifts movement mechanics to the deltoid muscle , compensating for rotator cuff dysfunction. 📈 Evidence Insight : According to a 2020 registry review, shoulder replacements have over 90% satisfaction rates and can last 15–20 years in many patients [1]. Signs It May Be Time for Shoulder Replacement Surgery Severe, Persistent Shoulder Pain: Pain that disrupts sleep, limits daily activities, or is present at rest may signal the need for surgical intervention. Advanced Shoulder Arthritis: X-rays and imaging may show joint space narrowing, bone-on-bone contact, bone spurs, or structural deformity of the joint, confirming arthritis progression. Stiffness and Limited Range of Motion: When conservative treatments no longer restore mobility, and everyday tasks like dressing, reaching overhead, or washing your hair become difficult, surgery may be the next step. Failed Non-Surgical Treatments: If medications, physiotherapy, injections, and activity modification no longer provide lasting relief, surgical intervention may offer more effective long-term outcomes. Large or Irreparable Rotator Cuff Tears: In cases where the rotator cuff is severely torn or no longer functioning (cuff tear arthropathy), a reverse shoulder replacement may be recommended to restore stability and function. When to Talk to a Specialist If shoulder pain has become a daily limitation, early referral for an orthopaedic evaluation is recommended. Dr Ryan du Sart will assess: Joint condition via physical exam and imaging Muscle integrity and rotator cuff status Your lifestyle, activity level , and treatment goals 📊 Clinical Note : Early assessment can often delay or optimise the timing of surgery. A 2021 study found patients undergoing surgery at the appropriate stage reported better functional outcomes and fewer complications [2]. What Does Recovery Look Like? Shoulder replacement is a major procedure, but outcomes are generally very positive when performed at the right time and followed by structured rehabilitation. Recovery timeline: 0–6 weeks: Shoulder supported in a sling; early physiotherapy to maintain motion 6–12 weeks: Gradual increase in active movement and strength 3–6 months: Return to light daily activities and driving 6–12 months: Full recovery for most patients, including return to recreation and improved sleep Dr du Sart and his team will support you throughout your recovery with tailored rehab plans and regular follow-up. Why Choose Dr Ryan du Sart Dr du Sart is an experienced orthopaedic surgeon with a patient-first approach, offering shoulder replacement surgery to patients throughout the South West of WA. With consulting rooms in Bunbury and Busselton , he provides local access to advanced orthopaedic care without the need to travel far from home. His focus is on: Evidence-based, personalised treatment Minimally invasive and joint-preserving techniques where possible Long-term outcomes and quality of life 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA References Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2020 . Saltzman BM, et al. Impact of surgical timing on outcomes in shoulder arthroplasty for osteoarthritis: A matched cohort study . J Shoulder Elbow Surg. 2021;30(5):1127–1135.

By Dr Ryan du Sart – Orthopaedic Surgeon, South West WA If you're preparing for orthopaedic surgery with Dr Ryan du Sart, it’s completely natural to feel a mix of anticipation and nerves. Understanding what will happen on the day of your procedure can ease anxiety, help you feel more confident, and ensure a smooth experience from arrival to discharge. Whether you're undergoing a joint replacement , arthroscopy , or foot and ankle surgery , this step-by-step guide outlines what to expect on your surgery day. 1. Before You Arrive In the days leading up to your procedure, you’ll receive detailed instructions from Dr du Sart’s team, including: Admission time and hospital location Fasting guidelines (typically no food or drink 6–8 hours prior to surgery) Medications to pause or continue What to bring: comfortable clothing, your hospital paperwork, Medicare and private health details If you’re using the mymobility® app, ensure your phone is charged and accessible—you’ll be able to track recovery milestones post-operatively. 2. Hospital Check-In Upon arrival at the hospital: You’ll check in with the admissions team A nurse will confirm your details, check vital signs, and prepare you for theatre An anaesthetist will meet with you to discuss your anaesthetic plan (general, spinal, or local) Dr du Sart will review the procedure with you and answer any last-minute questions You’ll be asked to change into a surgical gown and remove any jewellery, nail polish, or contact lenses. 3. Heading to the Operating Theatre When it’s time for your surgery: You’ll be taken to the pre-operative area A member of the surgical team will guide you into the operating theatre Anaesthesia is administered under close monitoring Dr du Sart will perform your surgery using modern, evidence-based techniques tailored to your condition Surgery times vary by procedure—for example, a knee arthroscopy may take under an hour, while a joint replacement can take 1.5–2 hours. 4. Waking Up in Recovery After surgery, you’ll be taken to the post-anaesthesia care unit (PACU) where: Nurses will monitor your vital signs, pain, and surgical site You may have a drip (IV) in place, and possibly a bandage, splint, or brace Pain will be managed using medications as needed Once you’re fully awake and stable, you’ll be transferred to your hospital room. 5. After Surgery: Your Hospital Stay Depending on your procedure, you may: Go home the same day (day surgery or minor procedures), or Stay overnight (e.g. for joint replacement or ligament repair) While in hospital: You’ll be encouraged to move (usually with assistance) as soon as possible Physiotherapists will visit to begin rehabilitation exercises You’ll receive post-operative instructions , including pain relief, wound care, and activity restrictions For joint replacements, the use of the Game Ready® system may also help reduce swelling and discomfort during the early recovery phase. 6. Going Home and Recovery Before discharge: You’ll be given a summary of your procedure Discharge instructions and follow-up appointments will be arranged Prescriptions for pain relief or anti-inflammatories will be provided You’ll receive guidance on when to resume walking, showering, and normal activities Expect a follow-up review with Dr du Sart typically 10–14 days after surgery. Depending on the surgery you’ve had you may be referred to the mymobility® app. This app will help guide your daily recovery with customised exercises, reminders, and educational content. Tips for a Smooth Experience ✅ Organise transport home in advance ✅ Arrange support for cooking, cleaning, and mobility if needed ✅ Follow medication and fasting instructions exactly ✅ Ask questions —our team is here to help ✅ Keep moving (within limits) after surgery to support circulation and healing You’re in Expert Hands Dr Ryan du Sart is committed to delivering high-quality orthopaedic care using modern, minimally invasive techniques and technology. With clinics in Bunbury and Busselton , we aim to make your surgical experience as safe, comfortable, and well-supported as possible. 📞 (08) 9779 9767 🌐 www.ryandusart.com.au 📍 South Bunbury & Busselton, WA Surgery can be a l ife-changing step toward pain relief and restored mobility. With the right preparation and support, your journey starts with confidence—and ends with better movement.