Knee
Knee Osteoarthritis
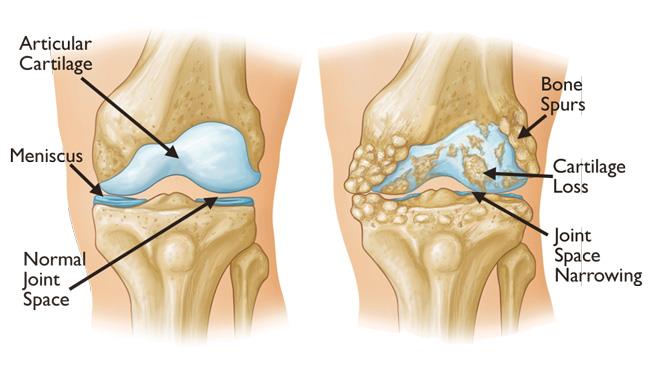
Knee osteoarthritis (OA) is a common degenerative condition that affects the knee joint. It occurs when the articular cartilage—the smooth cushioning tissue in the knee—gradually breaks down. This leads to pain, stiffness, inflammation, and restricted movement in the knee joint. As the cartilage deteriorates, the bones in the knee begin to rub against each other, causing further damage.
The knee joint consists of three main bones: the femur (thigh bone), tibia (shin bone), and patella (kneecap). In a healthy knee, the cartilage acts as a cushion and allows smooth, frictionless movement. When osteoarthritis sets in, it impacts these structures and leads to significant joint discomfort.
Causes and Risk Factors
While the exact cause of knee osteoarthritis is not always known, several factors contribute to the development of the condition:
- Advancing Age: The risk of osteoarthritis increases with age, as the cartilage in the knee wears down over time.
- Injury: Previous knee injuries or fractures, such as a torn ligament or meniscus damage, can increase the likelihood of osteoarthritis.
- Obesity: Excess weight places additional stress on the knee joint, accelerating cartilage breakdown. Studies show that each additional 5 kg of weight increases the risk of OA by 36% in weight-bearing joints .
- Genetics: A family history of osteoarthritis can increase the likelihood of developing the condition.
- Overuse: Repetitive use of the knee in high-impact activities or occupations that involve frequent bending or kneeling can contribute to OA development.
According to the Australian Institute of Health and Welfare (2023), knee osteoarthritis is one of the leading causes of disability in older adults, affecting approximately 1 in 7 Australians over the age of 65 .
Symptoms of Knee Osteoarthritis
Knee osteoarthritis often develops gradually, and the severity of symptoms can range from mild discomfort to debilitating pain. Common symptoms include:
- Pain: Often felt during or after activity, especially while walking, climbing stairs, or standing for prolonged periods.
- Stiffness: The knee may feel stiff, particularly after sitting for long periods or in the morning.
- Swelling and Inflammation: The knee may appear swollen or feel warm to the touch.
- Limited Range of Motion: Difficulty in fully bending or straightening the knee.
- Weakness: Muscle weakness around the knee can result from reduced movement or pain.
- Instability: A feeling that the knee may "give way," making it difficult to bear weight on the joint.
- Over time, these symptoms can interfere with daily activities and lead to difficulty walking, climbing stairs, and performing normal tasks like getting in and out of a chair.
Diagnosis of Knee Osteoarthritis
Diagnosing knee osteoarthritis typically involves a clinical examination, where Dr. Ryan du Sart will assess your medical history, symptoms, and perform physical tests to evaluate knee function. Imaging tests such as X-rays are commonly used to determine the severity of cartilage loss, joint space narrowing, and the presence of osteophytes (bone spurs).
In some cases, an MRI may be used to assess soft tissue damage or early-stage osteoarthritis when X-rays are inconclusive. Accurate diagnosis is critical for devising an effective treatment plan and managing symptoms before the condition progresses.

Treatment Options for Knee Osteoarthritis
While there is no cure for osteoarthritis, several treatment options can help manage symptoms, reduce pain, and maintain function in the knee joint.
Non-Surgical Treatments (Conservative Care)
For early-stage OA or patients who are not ready for surgery, non-operative treatments can be very effective. The most common approaches include:
- Weight Management: Reducing excess weight can significantly relieve stress on the knee joint and help improve function .
- Physical Therapy: Strengthening the muscles around the knee, improving flexibility, and practicing joint stability exercises can reduce pain and improve mobility .
- Medication: NSAIDs (non-steroidal anti-inflammatory drugs) like ibuprofen can help reduce inflammation, while paracetamol can alleviate pain. Topical treatments and joint injections may also be used.
- Exercise: Low-impact activities such as swimming, cycling, or Pilates can help strengthen muscles without putting undue stress on the knee joint .
- Corticosteroid Injections: In some cases, corticosteroid injections can provide short-term pain relief and reduce inflammation.
Surgical Treatment
Total Knee Replacement (TKR)
When symptoms no longer respond to conservative measures, surgery may be recommended. The most common surgical treatment for advanced knee osteoarthritis is Total Knee Replacement (TKR).
- Total Knee Replacement involves removing the damaged cartilage and bone from the knee joint and replacing them with prosthetic components made from metal, ceramic, and plastic. This procedure restores knee function and significantly improves pain and mobility .
A study by the Australian Orthopaedic Association (AOA, 2022) found that 95% of patients report significant improvement in pain and function at 5 years post-surgery .
Partial Knee Replacement (Unicompartmental Knee Replacement)
In some cases, knee osteoarthritis affects only one part of the knee joint. For patients with isolated cartilage damage, a partial knee replacement may be recommended, which only replaces the damaged area. This can allow for a more "natural" feeling knee post-surgery.
Knee Arthroscopy
Knee arthroscopy is typically used in earlier stages of osteoarthritis, particularly for patients with joint problems other than cartilage degeneration. While arthroscopy can clean up damaged tissue, it is not typically a long-term solution for advanced OA.
Osteotomy (Knee Realignment Surgery)
In younger patients or those with knee OA confined to one compartment, osteotomy may be recommended. This involves cutting and realigning the bone to shift the load from the damaged area of the knee joint, alleviating pain and preventing further damage.
Recovery and Rehabilitation
Post-surgery recovery varies depending on the type of treatment. Non-surgical treatments generally involve:
- Rest and Activity Modification: Reducing high-impact activities and focusing on low-impact exercises.
- Physical Therapy: Rehabilitation exercises to restore strength and mobility are critical for improving function.
- Gradual Weight-Bearing: Depending on the severity of the injury and type of treatment, most patients can begin resuming normal activities within 3-6 months.
After knee replacement surgery, patients can expect a recovery period of 3-6 months, with full rehabilitation lasting up to 12 months.
Preventing Knee Osteoarthritis Progression
While knee osteoarthritis (OA) is progressive, there are several steps you can take to manage symptoms and slow its progression:
- Maintain a Healthy Weight: Reducing excess weight decreases the strain on your knee joints, helping to slow OA progression. Studies show that losing even a small amount of weight can significantly reduce joint pain and improve mobility.
- Exercise Regularly: Engage in low-impact exercises such as swimming, cycling, and walking to strengthen the muscles around your knee. Physiotherapy exercises are also recommended to maintain joint function and alleviate pain.
- Footwear: Wear shoes with proper support and cushioning to reduce joint stress during physical activities. Avoid high heels or poorly fitting shoes, which can exacerbate knee pain.
- Activity Modifications: Modify activities to reduce knee stress. Avoid high-impact exercises and focus on low-impact activities, such as cycling or swimming, to maintain joint function.
- Medications & Injections: Pain relief medications, such as NSAIDs, can reduce inflammation and pain. In some cases, corticosteroid injections may offer short-term relief and allow you to remain active.
- Preventative Measures: Strengthening the muscles around the knee, using braces or supports during activity, and avoiding sudden increases in exercise intensity can help protect your knee and prevent further damage.
Why Choose Dr. Ryan du Sart?
Dr. Ryan du Sart is a highly experienced, fellowship-trained orthopaedic surgeon specialising in knee osteoarthritis treatment. His expertise includes total knee replacement surgery, partial knee replacements, and minimally invasive techniques. Dr. du Sart is committed to providing personalised, evidence-based care to improve your mobility and quality of life.
Book a Consultation
If you’re struggling with knee pain or symptoms of osteoarthritis, early intervention is key to better outcomes. Book a consultation with Dr. Ryan du Sart today.
Phone: (08) 9779 9767
Email:
admin@ryandusart.com.au
Clinic Locations:
6 Higgins Street, South Bunbury, WA 6230
20 Prince Street, Busselton, WA 6280
References:
- Felson D, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum [Internet]. 1998 Aug;41(8):1343-55.
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull WHO [Internet]. 2003 Nov 14;81(9):646-56.
- Fransen M, et al. Exercise for osteoarthritis of the hip. Cochrane Review. 2020.
- Bannuru RR, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019.
- Learmonth ID, et al. The operation of the century: total hip replacement. Lancet. 2007.
- AOANJRR Annual Report. Australian Orthopaedic Association National Joint Replacement Registry. 2022.