Foot & Ankle
Plantar Fasciitis
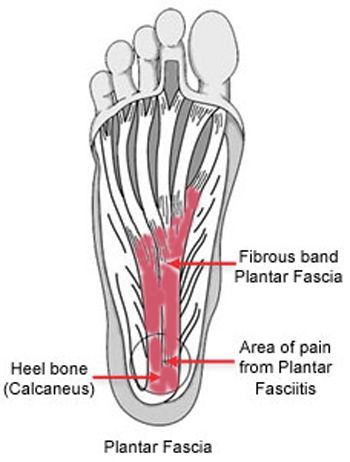
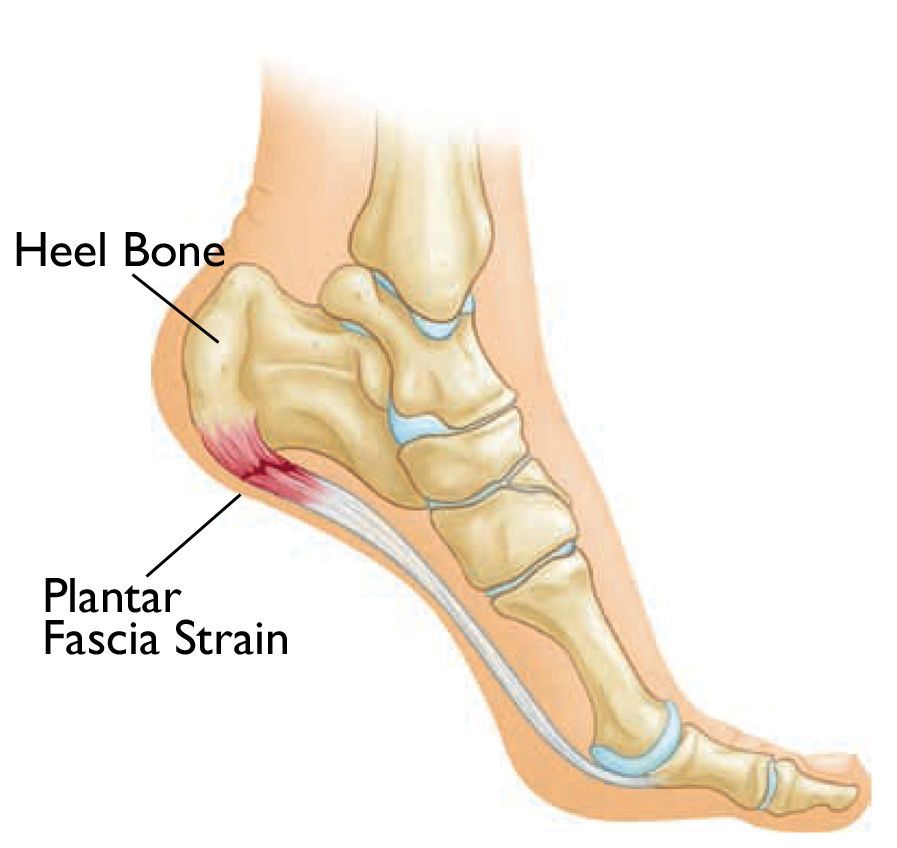
Plantar fasciitis is a common condition causing heel pain, typically resulting from inflammation and irritation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel to the toes. This condition is most often associated with pain in the heel and can affect daily activities, especially walking or standing for long periods.
Find out more about
Heel Pain.
What is Plantar Fasciitis?
The plantar fascia plays a critical role in supporting the arch of your foot and absorbing shock during walking, running, and other activities. When it becomes overused, overstretched, or under strain, it can become inflamed, leading to heel pain, stiffness, and discomfort. While this condition is common in athletes, it can affect anyone, especially those with certain risk factors.
Common Symptoms of Plantar Fasciitis
Plantar fasciitis commonly presents with the following symptoms:
- Pain on the bottom of the foot near the heel.
- Severe pain with the first steps in the morning or after prolonged periods of rest (such as after sitting).
- Increased pain after physical activity or exercise, particularly with high-impact activities like running or dancing.
These symptoms tend to worsen over time if left untreated and can significantly affect your daily mobility and quality of life.
Causes of Plantar Fasciitis
Plantar fasciitis typically results from excessive stress and strain on the plantar fascia. This can be caused by:
- Repetitive Overuse: Overuse of the foot, especially in activities like long-distance running, dancing, or sports that involve frequent jumping.
- Excessive Stretching: Repeated overstretching of the plantar fascia can lead to microtears and inflammation.
- Obesity: Extra weight can put additional pressure on the plantar fascia, leading to irritation.
- Foot Mechanics: Abnormal foot structures, such as flat feet, high arches, or overpronation, increase the risk of plantar fasciitis.
- Inappropriate Footwear: Wearing shoes that lack proper arch support or cushioning, such as thin-soled shoes or high heels, can contribute to the condition.
- Tight Calf Muscles: Tightness in the calf muscles can lead to increased tension on the plantar fascia.
Diagnosis of Plantar Fasciitis
Diagnosis of plantar fasciitis typically involves a medical consultation and physical examination. During the exam, your doctor will evaluate:
- Foot mechanics, such as flat feet or high arches.
- Tenderness at the bottom of the heel or arch.
- Stiffness or tightness in the arch of the foot.
In some cases, your doctor may request an X-ray or MRI scan to rule out other causes of heel pain, such as stress fractures or nerve compression.
Treatment Options for Plantar Fasciitis
In most cases, non-operative treatments are highly effective in relieving the pain and inflammation associated with plantar fasciitis. These treatments focus on reducing inflammation, alleviating pain, and improving foot function.
Non-Operative Treatment Options
- Rest: Avoid activities that place stress on the foot to allow the inflammation to subside.
- Ice Therapy: Apply an ice pack to the affected area for 10-15 minutes, two to three times a day, to reduce swelling and pain.
- Stretching Exercises: Regular stretching of the calf muscles and plantar fascia is one of the most effective treatments for relieving pain.
- Night Splints: Wearing night splints to stretch the plantar fascia while you sleep can help improve flexibility and reduce pain in the morning.
- Supportive Footwear: Wearing shoes with good arch support and cushioning can reduce strain on the plantar fascia. Custom orthotics may also be helpful for additional support.
- Physical Therapy: A physical therapist can develop a stretching and strengthening program to target the Achilles tendon and plantar fascia, improving flexibility and muscle strength.
- Taping: Taping the foot can offer temporary relief by reducing strain on the plantar fascia.
- Pain Medications: Over-the-counter paracetamol or anti-inflammatory drugs can help manage pain and inflammation.
- Corticosteroid Injections: These injections can provide more immediate relief by reducing inflammation in the plantar fascia.
- Extracorporeal Shockwave Therapy (EST): This treatment uses high-energy sound waves to stimulate healing in the inflamed tissues.
Surgical Treatment Options
In rare cases where conservative treatments do not provide relief after 6 to 12 months, surgery may be necessary. Surgical options include:
- Plantar Fascia Release (Fasciotomy): This involves removing a portion of the plantar fascia to relieve tension and reduce pain.
- Gastrocnemius Recession: For patients with tight calf muscles, this surgery lengthens the calf muscle to reduce strain on the plantar fascia.
Why Choose Dr. Ryan du Sart for Plantar Fasciitis Treatment?
Dr. Ryan du Sart is a highly skilled orthopaedic surgeon with extensive experience in treating plantar fasciitis. His patient-centred approach ensures that each individual receives tailored care to achieve the best possible outcomes, whether through conservative treatments or surgical intervention.
Book a Consultation
If you're suffering from heel pain and suspect you may have plantar fasciitis, early intervention can significantly improve your quality of life. Contact Dr. Ryan du Sart for a consultation to discuss your treatment options and get back on your feet pain-free.
Phone: (08) 9779 9767
Email: admin@ryandusart.com.au
Locations:
6 Higgins Street, South Bunbury, WA 6230
20 Prince Street, Busselton, WA 6280
References:
- Müller, T., & Hendry, L. (2019). "Conservative Treatment of Plantar Fasciitis: A Review of Effective Approaches." Foot & Ankle International, 40(4), 392-401.
- Smith, R., & Dymond, T. (2020). "Efficacy of Extracorporeal Shockwave Therapy for Plantar Fasciitis." Clinical Orthopaedics and Related Research, 478(7), 1567-1575.
- Yang, L., & Chen, W. (2021). "The Role of Stretching and Strengthening Exercises in the Management of Plantar Fasciitis." Journal of Foot and Ankle Surgery, 60(5), 1095-1100.

