FOOT & ANKLE
Ankle Sprain & Ligament Injury
Ankle sprains and ligament injuries are among the most common injuries seen in people of all ages and activity levels. An ankle sprain occurs when the ligaments that support the ankle joint are stretched or torn due to a sudden movement, fall, or awkward landing.
Understanding Ankle Sprains
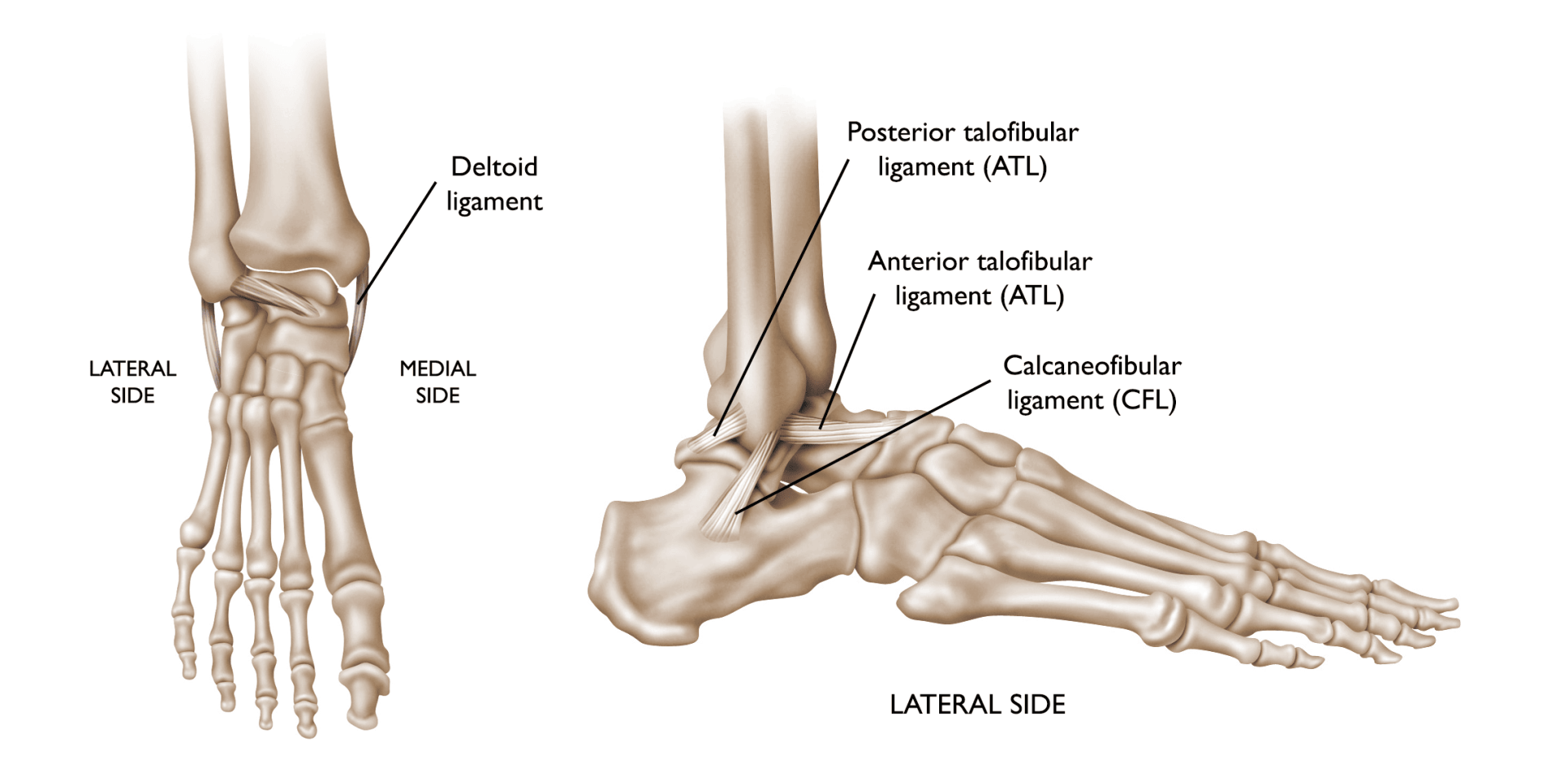
About 90% of ankle sprains involve an inversion injury, where the foot turns inward, damaging the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL) – the lateral ligaments on the outside of the ankle. In more severe cases, a "high-ankle sprain" may occur, affecting the syndesmotic ligaments or the medial (deltoid) ligament on the inside of the ankle.
Ankle sprains are a common orthopaedic injury, especially among athletes and active individuals. According to the American Orthopaedic Foot & Ankle Society (2020), sprains account for up to 25% of all sports-related injuries. If not treated properly, an ankle sprain can lead to chronic instability, repeated injuries, and long-term complications such as osteoarthritis.
These injuries are typically the result of a sudden twisting motion—such as landing awkwardly, changing direction quickly, or stepping on an uneven surface. Sports such as basketball, netball, soccer, and trail running often contribute to ankle sprains, though they can also occur in everyday activities.
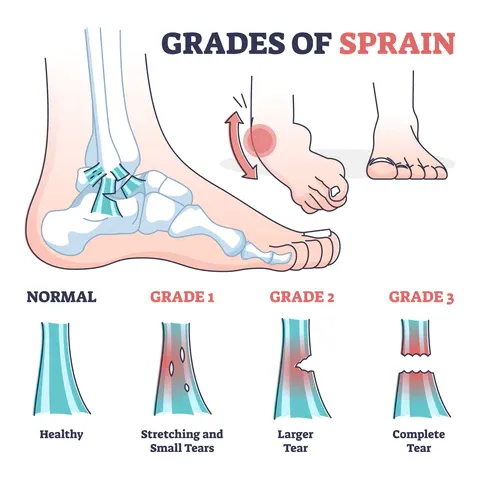
Ankle sprains range in severity:
Grade I (mild): Slight stretching or micro-tearing of the ligament fibres.
Grade II (moderate): Partial tearing of the ligament with some joint instability.
Grade III (severe): Complete rupture of the ligament, resulting in significant instability.
If left untreated or inadequately managed, ankle sprains can lead to chronic ankle instability, repeated injuries, and long-term joint issues such as arthritis.
Causes and Risk Factors
Ankle sprains often result from sudden movements or forces that cause the ankle to move beyond its normal range. Common causes include:
- Sports Injuries: Sports that require running, jumping, or sudden changes in direction, such as basketball, football, and soccer, are common causes of ankle sprains.
- Falls or Twists: Missteps while walking, tripping on uneven surfaces, or slipping on wet ground can cause the ankle to twist and sprain.
- Sudden Increase in Activity: A sudden increase in physical activity, especially without adequate conditioning or warm-up, can overload the ankle joint and lead to a sprain.
- Weak or Imbalanced Muscles: Weakness in the ankle or lower leg muscles, or poor proprioception (balance) can increase the risk of injury.
- Inadequate Footwear: Shoes that do not provide adequate support or fit improperly can contribute to sprains by destabilising the ankle.
Symptoms of Ankle Sprains
The symptoms of an ankle sprain vary depending on the severity of the injury but typically include:
- Pain: Pain at the site of the sprain, particularly on the outside of the ankle.
- Swelling and Bruising: Noticeable swelling and bruising around the ankle joint, which can occur immediately or develop over time.
- Inability to Bear Weight: Difficulty walking or standing on the affected foot due to pain and instability.
- Deformity: In more severe sprains, visible misalignment or deformity of the ankle joint can occur.
- Instability: A feeling that the ankle is “giving way” or buckling, especially when walking or bearing weight.
If you experience any of these symptoms after an injury, it's important to seek medical attention promptly to avoid complications and ensure proper treatment.
Diagnosis of Ankle Sprains
Dr. Ryan du Sart will conduct a thorough clinical assessment to determine the extent of the injury. This will include examining the injured area, assessing for pain, swelling, and deformity, and evaluating the range of motion in the affected joint. Imaging studies may be necessary to confirm the diagnosis and rule out associated injuries such as fractures:
- X-rays: An essential first step to ensure no fractures are present and to assess for any bone damage.
- MRI: In cases of more severe ligament tears or if soft tissue damage (such as tendon involvement) is suspected, an MRI may be used for a more detailed evaluation of the injury.
- Ultrasound: Sometimes used to assess the extent of soft tissue damage, including ligament tears and swelling around the ankle.
Treatment Options for Ankle Sprains
Dr. Ryan du Sart offers a range of treatment options based on the severity of the sprain and the patient's needs. These options may include conservative non-surgical treatments or surgical intervention for more severe injuries.
Non-Surgical Treatment (Grade I & II Sprains)
For most mild to moderate sprains (Grade I and II), non-surgical treatment is effective and typically includes:
- RICE Protocol: Rest, Ice, Compression, and Elevation in the first 48–72 hours to reduce swelling, manage pain, and accelerate recovery.
- Immobilisation: The use of a walking boot, brace, or splint to keep the ankle immobilised and prevent further injury during the healing process.
- Pain Management: Pain relievers such as paracetamol or NSAIDs (non-steroidal anti-inflammatory drugs) are commonly prescribed to manage pain and reduce inflammation.
- Physical Therapy: Once the initial pain and swelling have subsided, physical therapy will focus on restoring strength, flexibility, and proprioception (balance). This will help prevent re-injury and improve recovery outcomes.
- Gradual Return to Activity: A structured and gradual return to sport or physical activity under medical supervision ensures the ankle has fully healed and is stable enough to bear weight without further damage.
Surgical Treatment (Grade III Sprains or Chronic Instability)
For severe sprains (Grade III), where the ligament is completely ruptured, or in cases of chronic ankle instability, surgery may be necessary. Surgical options include:
- Lateral Ligament Reconstruction: This involves repairing or reconstructing the ATFL and CFL ligaments to restore stability and prevent recurrent sprains.
- Arthroscopic Surgery: In some cases, arthroscopy may be used to clean out the joint or repair damaged tissues within the ankle joint.
- Ankle Stabilisation Surgery: For patients with severe instability, a more extensive surgery may be required to stabilise the ankle and ensure long-term joint function.
Dr. du Sart will discuss the most appropriate surgical approach based on the severity of your injury, your goals, and your overall health.
When Is Surgery Required?
In cases of chronic ankle instability, recurrent sprains, or complete ligament rupture where non-operative treatment has not been successful, surgical intervention may be recommended.
Lateral ligament reconstruction is the most common surgical procedure for chronic instability. This involves repairing or reconstructing the ATFL and CFL ligaments to restore stability to the ankle. Surgical treatment may also be considered when there are associated injuries, such as cartilage lesions or tendon involvement that require direct intervention.
Recovery and Rehabilitation
Recovery from an ankle sprain can take several weeks, depending on the severity of the injury and the treatment method. A typical recovery process involves:
- Initial Rest and Immobilisation: After an ankle sprain, the injured foot will be immobilised to allow the ligaments time to heal. This typically involves a cast, boot, or brace.
- Physical Therapy: A structured rehabilitation program will help restore range of motion, strength, and balance. It is critical to follow the physical therapy plan to ensure a full recovery and reduce the risk of long-term complications.
- Gradual Weight-Bearing: As the ankle heals, weight-bearing activities can be gradually introduced, with full activity typically resumed after 4–6 weeks for mild sprains and 6–8 weeks for more severe sprains.
- Return to Sports: Athletes can generally return to their regular activities in 6–8 weeks, depending on the severity of the sprain and rehabilitation progress.
Preventing Future Ankle Sprains
Preventing future ankle sprains is crucial, especially for individuals who have previously injured their ankle. Strategies include:
- Rehabilitation Completion: Always complete your rehabilitation program, even after pain subsides, to prevent re-injury.
- Footwear: Wear supportive footwear that offers adequate stability, especially during physical activities or sports.
- Balance and Proprioception Exercises: Strengthening exercises, balance training, and proprioception exercises can help improve ankle stability and reduce the risk of sprains.
- Ankle Bracing or Taping: In high-risk sports, using ankle braces or taping can provide extra support and protection for the ligaments during activity.
Why Choose Dr. Ryan du Sart?
Dr. Ryan du Sart is a highly experienced orthopaedic surgeon with a special interest in foot and ankle injuries. His patient-first approach ensures that every treatment plan is customised to meet the individual needs of each patient. Whether you have a mild sprain or require surgical intervention, Dr. du Sart uses the latest techniques to optimise recovery and get you back to your normal activities.
Book a Consultation
If you've sustained an ankle sprain or are experiencing recurring ankle instability, don’t wait to seek professional medical care. Early intervention can significantly reduce the risk of long-term complications.
Phone: (08) 9779 9767
Email: admin@ryandusart.com.au
Locations:
6 Higgins Street, South Bunbury, WA 6230
20 Prince Street, Busselton, WA 6280
References:
- American Orthopaedic Foot & Ankle Society (AOFAS). (2021). Ankle sprain and ligament injuries.https://www.aofas.org
- Cleveland Clinic. (2020). Ankle sprain treatment.https://my.clevelandclinic.org/health/diseases/15298-ankle-sprain
- British Journal of Sports Medicine (BJSM). (2018). Ankle sprain rehabilitation.https://bjsm.bmj.com
- Royal Australian College of Surgeons (RACS). (2020). Management of ankle sprains.https://www.surgeons.org

